Healthcare costs continue to rise across the United States, making quality medical care increasingly difficult for millions of Americans to afford. In this challenging landscape, Medicaid serves as a crucial lifeline, providing essential healthcare coverage to those who need it most. Whether you’re navigating the system for the first time or trying to understand recent changes, this comprehensive guide will help you understand everything you need to know about Medicaid.
What is Medicaid?
Medicaid is a joint federal and state program that provides healthcare coverage to eligible low-income individuals and families. Unlike Medicare, which primarily serves seniors, Medicaid covers people of all ages, including children, pregnant women, elderly adults, and people with disabilities. The program is designed to ensure that financial barriers don’t prevent Americans from accessing essential medical care.
Key Medicaid Facts:
- Established: 1965 as part of the Social Security Act
- Current Coverage: Over 80 million Americans
- Funding: Joint federal-state partnership
- Scope: Largest source of healthcare funding for low-income Americans
- Administration: Run by states with federal oversight
Who Does Medicaid Cover?
- Low-income families with children
- Pregnant women
- Elderly adults (65+)
- People with disabilities
- Children in foster care
- Some low-income adults (in expansion states)
State-Specific Medicaid Programs: What’s in a Name?
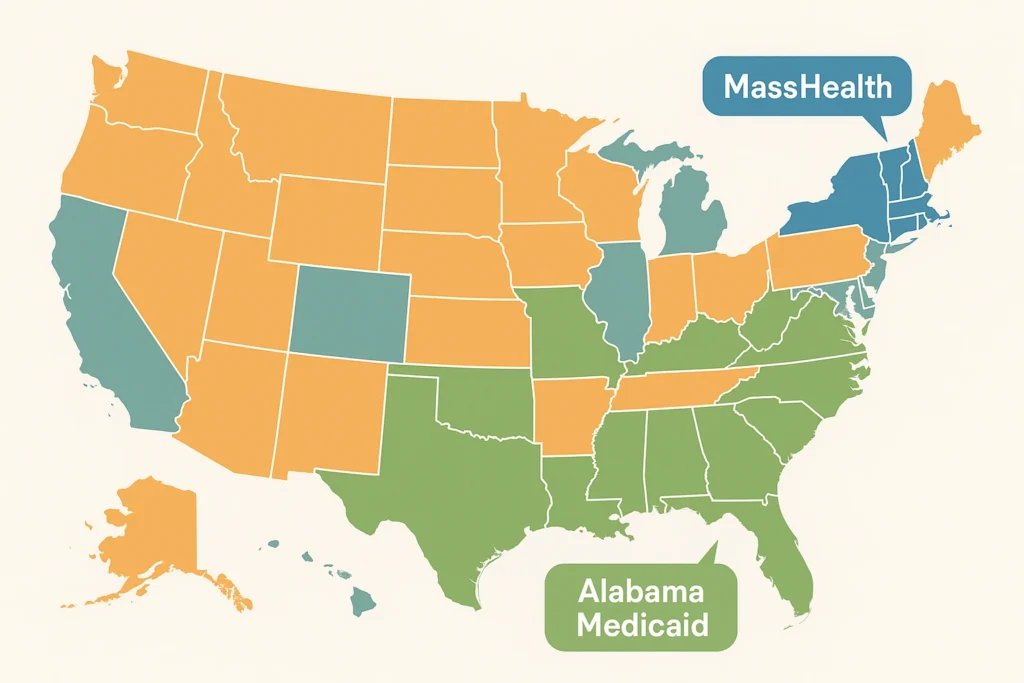
One of the most confusing aspects of Medicaid is that different states often give their programs unique names. This branding strategy helps states tailor their messaging and make the program feel more locally relevant to residents.
| State | Program Name | Special Features |
|---|---|---|
| Massachusetts | MassHealth | Comprehensive coverage, innovative delivery models |
| Alabama | Alabama Medicaid | Traditional structure, exploring modernization |
| California | Medi-Cal | Largest state program, extensive benefits |
| New York | Medicaid | Enhanced community services |
| Texas | Texas Medicaid | Fee-for-service model |
| Florida | Florida Medicaid | Managed care focus |
What is Medicaid Called in Massachusetts?
In Massachusetts, Medicaid is called MassHealth. This program has been particularly notable for its comprehensive coverage and innovative approaches to healthcare delivery.
MassHealth Coverage Types:
- Standard: Basic coverage for low-income individuals and families
- CommonHealth: For people with disabilities who work
- CarePlus: For people who need long-term care services
- Family Assistance: Premium assistance for employer-sponsored insurance
Services Covered by MassHealth:
- Doctor visits and specialist care
- Hospital inpatient and outpatient services
- Prescription medications
- Mental health and substance abuse treatment
- Dental care (comprehensive for children, limited for adults)
- Vision care and eyeglasses
- Medical equipment and supplies
- Transportation to medical appointments
What is Medicaid Called in Alabama?
Alabama’s Medicaid program operates under the official name Alabama Medicaid. Unlike some states that have adopted catchier brand names, Alabama has maintained the traditional Medicaid designation.
Alabama Medicaid Key Features:
- Administration: Alabama Department of Public Health
- Coverage: Essential health services for eligible residents
- Model: Primarily fee-for-service with some managed care elements
- Expansion Status: Has not expanded under the Affordable Care Act
Recent Changes and Developments
The Medicaid landscape has been particularly dynamic in recent years, with several significant changes affecting beneficiaries across the country.
What Part of Medicaid is Being Cut?
Recent policy discussions have focused on various aspects of Medicaid funding and coverage. While specific cuts vary by state and federal policy changes, several areas have been subject to scrutiny:
Areas Experiencing Reductions or Changes:
| Area of Change | Impact | States Affected |
|---|---|---|
| Work Requirements | Mandatory employment/training for some beneficiaries | Arkansas, Kentucky, others |
| Provider Payment Rates | Reduced payments to healthcare providers | Multiple states |
| Coverage Redeterminations | Regular eligibility reviews resumed | All states |
| Optional Services | Cuts to dental, vision, or therapy services | State-specific |
| Administrative Costs | Reduced funding for program administration | Various states |
Specific Changes Include:
- Work Requirements: Some states have implemented requirements that certain beneficiaries work or participate in job training programs to maintain coverage
- Provider Payment Reductions: Lower reimbursement rates for healthcare providers, potentially affecting service availability
- “Unwinding” Process: Resume of regular eligibility reviews after COVID-19 pause, leading to some coverage losses
- Service Limitations: Restrictions on adult dental care, vision services, or specific therapy types in some states
- Administrative Efficiency: Streamlined processes that may reduce access for some beneficiaries
What Are the New Medicaid Requirements?
Recent years have brought several new requirements and changes to Medicaid programs across the country:
New Program Requirements:
| Requirement Type | Description | Implementation Timeline |
|---|---|---|
| Enhanced Reporting | Detailed quality metrics and spending data | Ongoing |
| Telehealth Services | Permanent remote healthcare access | 2023-2024 |
| Mental Health Parity | Equal coverage for mental and physical health | Ongoing |
| Care Coordination | Better provider communication systems | 2023-2025 |
| Fraud Prevention | Advanced detection technologies | Ongoing |
| Community Health Workers | Coverage for community-based services | State-specific |
Key New Requirements:
- Enhanced Transparency: States must provide more detailed reporting on program performance, including quality metrics and beneficiary outcomes
- Telehealth Expansion: Permanent coverage for remote healthcare services, accelerated by COVID-19 pandemic
- Mental Health Integration: Increased emphasis on parity between mental health and physical health services
- Improved Care Coordination: New systems for better communication between healthcare providers and services
- Advanced Fraud Detection: Implementation of new technologies to identify and prevent program fraud
- Community Health Worker Coverage: Recognition and payment for services provided by community health workers
- Quality Measurement: Enhanced focus on measuring and reporting healthcare outcomes and patient satisfaction
Understanding Medicaid Eligibility
Medicaid eligibility varies significantly by state, but there are some general guidelines that apply across most programs. Eligibility is primarily based on income, household size, and specific circumstances such as pregnancy, disability, or age.
Federal Poverty Level Guidelines (2024):
| Household Size | 100% FPL | 138% FPL (Expansion) | 200% FPL |
|---|---|---|---|
| 1 person | $15,060 | $20,783 | $30,120 |
| 2 people | $20,440 | $28,207 | $40,880 |
| 3 people | $25,820 | $35,631 | $51,640 |
| 4 people | $31,200 | $43,056 | $62,400 |
| 5 people | $36,580 | $50,480 | $73,160 |
Medicaid Expansion Status by State:
Expansion States (39 + DC):
- Full Expansion: California, New York, Massachusetts, Illinois, Pennsylvania, Ohio, Michigan, and 32 others
- Recent Expansion: Montana (2016), Louisiana (2016), Maine (2019), Idaho (2020), Utah (2020), Nebraska (2020), Oklahoma (2021), Missouri (2021)
Non-Expansion States (12):
- Alabama, Florida, Georgia, Kansas, Mississippi, North Carolina, South Carolina, South Dakota, Tennessee, Texas, Wisconsin, Wyoming
Eligibility Categories:
- Mandatory Groups: Children, pregnant women, elderly, disabled individuals
- Optional Groups: Low-income adults (in expansion states), medically needy individuals
- Special Circumstances: Foster care youth, Medicare beneficiaries, emergency services for undocumented immigrants
The Importance of Medicaid in Healthcare Access
Medicaid plays a crucial role in ensuring healthcare access for vulnerable populations. The program covers a comprehensive range of services that are essential for maintaining health and treating illness.
Core Medicaid Services:
| Service Category | Included Services | Coverage Details |
|---|---|---|
| Medical Services | Doctor visits, specialist care, hospital stays | Inpatient and outpatient care |
| Diagnostic Services | Laboratory tests, X-rays, MRI, CT scans | Medically necessary testing |
| Prescription Drugs | Medications, medical supplies | State formularies vary |
| Mental Health | Therapy, counseling, psychiatric care | Parity with physical health |
| Preventive Care | Screenings, vaccinations, wellness visits | Focus on early detection |
| Long-term Care | Nursing homes, home health services | Largest payer of long-term care |
Medicaid’s Impact by the Numbers:
- Coverage: 1 in 5 Americans rely on Medicaid
- Births: Medicaid covers 40% of all births in the US
- Children: 37% of children are covered by Medicaid/CHIP
- Nursing Home Care: Medicaid pays for 62% of nursing home residents
- Rural Healthcare: Critical funding source for rural hospitals
- Mental Health: Largest payer of mental health services
Essential Services Covered:
- Emergency Services: 24/7 emergency room care and ambulance services
- Family Planning: Contraception, reproductive health services
- Maternity Care: Prenatal, delivery, and postpartum care
- Pediatric Services: Comprehensive child healthcare including EPSDT
- Rehabilitative Services: Physical therapy, occupational therapy, speech therapy
- Dental Care: Comprehensive for children, emergency for adults (varies by state)
- Vision Care: Eye exams, glasses, treatment for eye diseases
- Transportation: Medical transportation to appointments
Addressing Public Interest and Concerns
The search trends shown in your Google Trends data reflect genuine public interest and concern about Medicaid. People are actively seeking information about their state’s programs, recent changes, and how policies might affect their coverage.
Top Medicaid Search Trends and What They Mean:
| Search Query | Search Volume Increase | What It Indicates |
|---|---|---|
| “What is Medicaid called in Massachusetts” | +2,000% | State-specific program confusion |
| “What happened to Jackson Cunningham” | +1,100% | Interest in individual impact stories |
| “What is Medicaid called in Alabama” | +700% | Regional program information needs |
| “What part of Medicaid is being cut” | +600% | Concern about program changes |
| “What are the new Medicaid requirements” | +500% | Need for current policy information |
Why “What Happened to Jackson Cunningham” is Trending
While specific individual cases like Jackson Cunningham might trend for various reasons, they often highlight broader issues within the Medicaid system. Such trending topics typically relate to:
Common Reasons for Individual Case Trends:
- Coverage Denials: Cases where individuals face unexpected coverage denials for necessary medical care
- Policy Impact Stories: Real-world examples of how policy changes affect beneficiaries
- System Navigation Challenges: Stories highlighting difficulties in accessing care or services
- Advocacy Efforts: Cases that become symbols for broader healthcare access issues
- Media Coverage: News stories that illustrate systemic problems through personal experiences
What These Stories Teach Us:
- Human Impact: Policy changes have real consequences for real people
- System Complexity: The difficulty many face in navigating Medicaid systems
- Coverage Gaps: Areas where current policies may not adequately serve beneficiaries
- Advocacy Importance: The role of individual stories in driving policy discussions
- Need for Support: The importance of assistance programs and advocacy organizations
Navigating the Medicaid System
For those who need to access Medicaid services, understanding how to navigate the system is crucial for getting the care you need.
Step-by-Step Application Process:
| Step | Action Required | Timeline | Tips |
|---|---|---|---|
| 1. Determine Eligibility | Check income and household size | Before applying | Use online pre-screening tools |
| 2. Gather Documents | Collect required paperwork | 1-2 weeks | Income, ID, residency proof |
| 3. Submit Application | Online, mail, or in-person | Same day | Apply online for fastest processing |
| 4. Interview (if required) | Phone or in-person interview | Within 30 days | Be prepared with all documents |
| 5. Receive Decision | Approval or denial notification | 45-90 days | Check status online regularly |
| 6. Activate Coverage | Receive Medicaid card | 1-2 weeks after approval | Keep card with you at all times |
Required Documentation Checklist:
- Identity: Driver’s license, state ID, or passport
- Income: Pay stubs, tax returns, unemployment benefits, Social Security statements
- Residency: Utility bills, lease agreements, mail with your address
- Household Size: Birth certificates, marriage certificates, custody papers
- Medical Information: For disability applications, medical records and doctor statements
- Immigration Status: For non-citizens, immigration documents
Understanding Medicaid Delivery Models:
Managed Care Organizations (MCOs):
- How It Works: You choose a health plan that coordinates your care
- Benefits: Care coordination, preventive focus, provider networks
- States Using MCOs: 40+ states use managed care for some or all services
- What You Need to Know: Choose a plan, select a primary care provider, understand your network
Fee-for-Service Model:
- How It Works: State pays providers directly for each service
- Benefits: More provider choice, direct payment system
- States Using FFS: Fewer states, mostly for certain services
- What You Need to Know: Find providers who accept Medicaid, understand covered services
Finding Healthcare Providers:
Provider Search Tips:
- Use State Directories: Every state maintains online provider directories
- Check Acceptance: Call provider offices to confirm they accept new Medicaid patients
- Understand Networks: In managed care states, stay within your plan’s network
- Consider Travel Time: Factor in transportation to appointments
- Ask About Services: Ensure providers offer the specific services you need
Types of Providers:
- Primary Care: Family doctors, internists, pediatricians
- Specialists: Cardiologists, endocrinologists, psychiatrists, etc.
- Facilities: Hospitals, clinics, urgent care centers
- Pharmacies: Those that accept Medicaid prescription coverage
- Mental Health: Therapists, counselors, psychiatric facilities
The Future of Medicaid

As healthcare costs continue to rise and the American population ages, Medicaid will likely play an increasingly important role in the healthcare system.
Emerging Trends and Future Developments:
| Trend | Description | Expected Timeline | Impact |
|---|---|---|---|
| Technology Integration | AI, telehealth, electronic health records | 2024-2027 | Improved efficiency and access |
| Value-Based Care | Payment based on outcomes, not volume | 2025-2030 | Better quality, cost control |
| Social Determinants | Addressing housing, food, transportation | 2024-2026 | Holistic health approach |
| Workforce Development | Training community health workers | 2024-2025 | Expanded access to care |
| Prevention Focus | Emphasis on wellness and early intervention | Ongoing | Reduced long-term costs |
Key Areas of Future Development:
Technology and Innovation:
- Artificial Intelligence: Improved fraud detection and care coordination
- Telehealth Expansion: Permanent remote care options, especially for rural areas
- Electronic Health Records: Better information sharing between providers
- Mobile Health Apps: Patient engagement and self-management tools
- Wearable Technology: Remote monitoring for chronic conditions
Policy and Funding Changes:
- Federal Funding Formulas: Potential changes to how federal matching funds are calculated
- Work Requirements: Ongoing legal and policy debates about employment mandates
- Expansion Discussions: Continued efforts to expand Medicaid in non-expansion states
- Integration with Other Programs: Better coordination with Medicare, SNAP, and housing assistance
- Long-term Care Reform: Addressing the growing need for aging population services
Healthcare Delivery Innovations:
- Community Health Centers: Expanded funding and services
- School-Based Health: Increased services in educational settings
- Pharmacy Integration: Enhanced medication management and counseling
- Mental Health Integration: Better coordination between physical and mental health services
- Specialized Programs: Targeted interventions for specific populations (e.g., pregnant women, people with disabilities)
Challenges and Opportunities:
Major Challenges:
- Rising Healthcare Costs: Balancing access with budget constraints
- Provider Shortages: Ensuring adequate healthcare workforce
- Administrative Complexity: Streamlining processes while maintaining oversight
- Political Pressures: Navigating changing federal and state priorities
- Health Disparities: Addressing inequities in care access and outcomes
Opportunities for Improvement:
- Preventive Care Emphasis: Reducing long-term costs through early intervention
- Care Coordination: Better integration of services across providers
- Community Partnerships: Leveraging local resources and organizations
- Data Analytics: Using information to improve program effectiveness
- Patient Engagement: Empowering beneficiaries to take active roles in their care
Understanding your state’s specific Medicaid program, staying informed about policy changes, and knowing how to navigate the system are all crucial for beneficiaries and their families. As the program continues to evolve, staying engaged with these changes and advocating for continued coverage will be important for maintaining this crucial healthcare safety net.
The trending searches reflected in recent Google data show that Americans are actively engaged with these issues, and this engagement is crucial for ensuring that Medicaid continues to serve its vital role in American healthcare. Whether you’re researching MassHealth in Massachusetts, Alabama Medicaid, or trying to understand new requirements and changes, the information in this guide provides a foundation for navigating the complex but essential world of Medicaid coverage.
Remember that if you need assistance with Medicaid applications or have questions about your coverage, most states offer customer service resources and local assistance programs to help you navigate the system effectively. Don’t hesitate to reach out for help – accessing healthcare is your right, and there are people and organizations available to help you exercise that right.






Leave a Comment